Meet three new faculty on the UMKC School of Dentistry team who are making an impact
By STACY DOWNS
The UMKC School of Dentistry has proven itself as an internationally known research powerhouse in the past decade, especially when it comes to studying bone and muscle deterioration as we all grow older, as well as possible remedies.
Three new researchers are studying what can make all ages heal — starting from in the womb — and treatments that could span the generations.
Correcting cleft palates
Timothy Cox’s research focuses on craniofacial birth defects.
Cox, professor and endowed chair of mineralized tissue research, focuses mostly on cleft palates. Children often undergo multiple surgeries to alleviate them. By multiple, we’re talking eight, nine or even 10 surgeries.
Cox was influenced to pursue this line of work while he was earning his doctorate. It was then he saw the severity of cleft palates in children.
The problem: it’s largely a mystery about what causes cleft palates. “Just because someone is genetically disposed to have one, doesn’t mean they get them,” Cox said.
Cox is investigating that there might be a link between cleft palates and maternal nutrition. Lacking vitamin A and consuming alcohol are among the risk factors. “We’re looking for interventional strategies to prevent cleft palates, particularly through diet modification in the mother,” Cox said.
In his lab, he’s training two undergraduates. He lectures dental students to provide insights into the latest data so they are aware of what’s going on in research that could affect their practice.
Cox doesn’t see patients directly — a pediatrician or clinical geneticist coordinates collections of samples and clinical summaries for his team to work with.
“That said, I find myself communicating with patients and families from time to time as they track me down and reach out with questions about their condition and wanting to volunteer for research studies,” he said.
Cox uses test models to find risk factors. Some of the risk factors have been suggested from clinical studies, but are difficult to prove in human cases because everything is so variable from person to person. However, once he and his colleagues have strong evidence for a risk factor and understand the conditions in which it becomes a risk factor, then their goal becomes working on a way to validate this better in a controlled clinical group.
“As excited as we may be to move everything to a population level as we get evidence in support of a risk factor, I think care must be taken not to rush into testing since we typically just test for positive effects on select groups in the first instance,” Cox said. “There should always be testing for negative effects and knowing the contexts in which they occur.”
 CAPTION: The work of Timothy Cox, PhD, often incorporates advanced quantitative 3D imaging.
CAPTION: The work of Timothy Cox, PhD, often incorporates advanced quantitative 3D imaging.
Timothy Cox, PhD
Professor and endowed chair of Oral and Craniofacial Sciences
Research Interests:
Genetics, cell biology and developmental biology that incorporates advanced quantitative 3D imaging. Current projects are focused on genetic and developmental mechanisms causing cleft lip /palate, midface hypoplasia and craniofacial microsomia.
Looking for less-invasive treatments for jaws
Erin Bumann is a licensed and board-certified pediatric dentist, but her research aims to solve problems far beyond what most children experience.
“Sometimes faces don’t form correctly, and these children can have issues with breathing, eating and speaking,” said Bumann, an assistant professor. “The only treatment currently available for these children is invasive surgery.”
The primary goal of her lab: identify nonsurgical methods to change the size and shape of the bones in the face, so these children either do not need to undergo surgery or need less invasive surgery.
To come up with methods for redirecting how the jaw and other facial bones grow and develop, Bumann’s laboratory works with test models. Her work already has indicated that the neural crest mesenchyme (NCM) cells control the activity of osteoclasts — other cells that resorb bone to shape the models’ developing jaw structures.
The hope is that Bumann’s discoveries eventually lead to therapies to correct or greatly lessen potential craniofacial problems. Such problems often can be detected by ultrasound, so therapies might be possible even in utero, much as surgeons now can correct or mitigate heart or spinal defects before birth. Therapies also could be effective throughout childhood, Bumann said, as much jaw and facial development occurs through adolescence.
Craniofacial abnormalities are one of the most common birth defects requiring invasive surgery, so alternative therapies could help thousands of children each year. Being able to better grow or re-grow facial bones also could help some accident victims and patients with cancer, Bumann said.
Buman was drawn to UMKC by the School of Dentistry’s research on bone mass and how bone and muscle cells “talk” with each other. A key part of that research involved osteocytes, once thought to be a relatively inactive part of bones.
“This department showed that osteocytes play a large role in bone formation, aging, a whole host of functions,” Bumann said.
It’s still widely believed that osteocytes aren’t active in utero, Bumann said, and her group is challenging that assumption, along with seeing how the NCM cells may regulate how the osteocytes, which come from NCM, form facial bones.
Bumann also loves working with and mentoring her lab crew. “I started in a research lab in my undergraduate training and it is why I am in the position I am in today. I think it is very important to give back and mentor future generations of scientists and dental professionals.”
In her short time at the School of Dentistry, Bumann already has made a difference. This year, the Kansas City Musculoskeletal Diseases Consortium made a nearly $50,000 grant for research Bumann will work on with a University of Kansas School of Medicine researcher. And she was selected for the 2019 Dr. David Whiston Leadership Award, established to provide formal leadership training for promising dentists early in their careers.
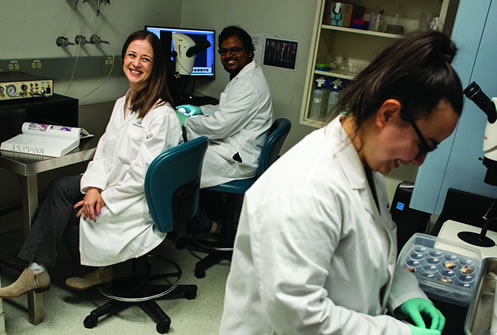
 CAPTION: Erin Bumann (left), PhD, DDS, MS, enjoys working with and mentoring
CAPTION: Erin Bumann (left), PhD, DDS, MS, enjoys working with and mentoring
student assistants in her lab.
Erin Bumann, PhD, DDS, MS
Assistant professor
Research Interests:
The role of neural crest mesenchyme (NCM) cells in regulating the formation of facial bones.
Engineering solutions
Other researchers covet the main tool in Stefan Lohfeld’s lab: a $250,000 top-notch 3D printer.
What Lohfeld makes with the printer can help people in many different ways. He creates scaffolds for tissue engineering at the Oral and Craniofacial Sciences Department at the School of Dentistry.
Scaffolds are being used in bone tissue engineering to provide a structure for the cells to grow on, to give them a direction and shape to grow into, and to provide temporary stability to the void where new bone needs to be generated. These scaffolds can be permanent — made of metal — or they can be biodegradable and be absorbed by the body as new bone is formed. The features of the scaffold, such as material, porosity and pore size, influence the tissue formation. Gradient scaffolds that provide various environments in different areas of the scaffold adapted to the several stages of tissue ingrowth can enhance the tissue formation dramatically.
With scaffolds, that’s where the primo printer comes into play. Its cartridges can print up to five materials in a single printing. It extrudes material in paste form, and its digital camera allows Lohfeld’s lab to document the printing of each layer. The printer has a sterile filter that allows for cell and organ printing.
Lohfeld concentrates on working with the acid PLGA, which is biodegradable and well-known for bone tissue engineering.
He eventually wants to enable delayed release of implanted drugs, he said, and to make scaffolds for bone and bone-cartilage tissue engineering for the mandible and the jaw joint. “The idea is to place different materials in different areas of the scaffold to enhance tissue growth and formation,” he said.
Using the same material and process as tissue-engineering scaffolds, he is collaborating with School of Medicine researchers on ophthalmological scaffold for the orbital floor.
Lohfeld also makes implants to help support the spine.
“The spine implant will make it easier for surgeons to implant large spinal instrumentation such as long rods along the spine to stabilize it, prevent movement for fusion or for shape corrections,” he said.
In keyhole surgery, which spares the patient from large scars and longtime pain during the healing phase of muscle tissue, surgeons have difficulties inserting long rods.
“My solution would address this issue, and it may have applications in both static and dynamic instrumentation by choosing how much it is tightened after insertion,” Lohfeld said.
Lohfeld also produces an access device for the carotid artery, enabling better instruments for stroke treatment — clot retrieval from the blood vessels in the brain — and for carotid-artery stenting. This makes the procedures faster, safer and likely cheaper by providing an in-built solution for protection from embolisms getting to the brain.
Lohfeld sees lots of potential solutions all around.
“I want to change materials, change the size, change the architecture and what it encapsulates,” Lohfeld said. “I want to play around with what is possible.”

CAPTION: Stefan Lohfeld, PhD, uses his 3D printer to make structures
such as scaffolds useful in bone tissue engineering research at the School of Dentistry.